The Dual Diagnosis Dilemma: Treating Addiction and Co-Occurring Mental Health Disorders
- Anmol Jeevan
- Nov 1, 2025
- 6 min read
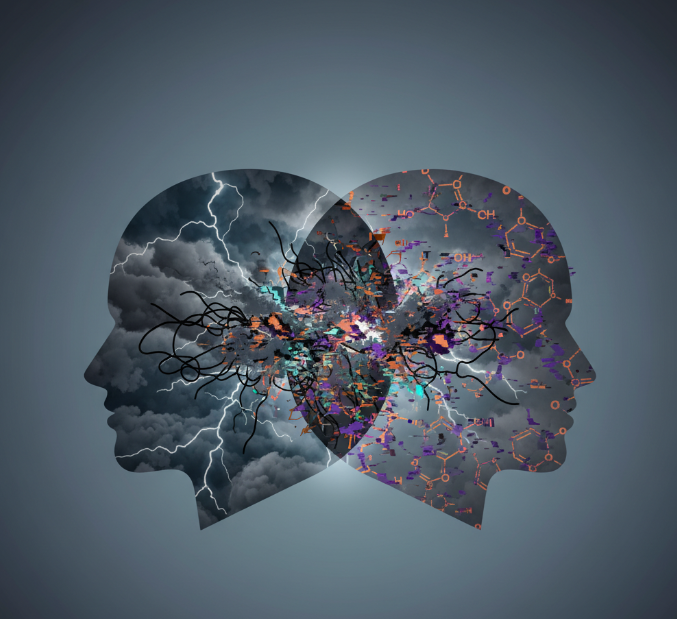
The path to recovery often begins with a single, courageous step: the decision to stop using a substance. It’s a moment of profound hope. But for many, the journey reveals a landscape far more complex than they first imagined. The silence left by addiction is soon filled with a familiar static—the persistent hum of anxiety, the heavy weight of depression, or the haunting echoes of past trauma. It becomes clear that the substance wasn't the only problem; in many cases, it was a symptom, a temporary shield against a deeper pain.
This is the reality of a dual diagnosis, a term that describes the co-occurrence of a substance use disorder (SUD) and a mental health disorder. It is not a rare exception; it is a common and challenging crossroads on the path to wellness.
At Anmol Jeevan Foundation, we believe that acknowledging and understanding this intersection is the first, most critical step toward building a recovery that is not just sustainable, but truly transformative. Untangling these intertwined conditions requires more than just willpower; it demands a compassionate, sophisticated, and integrated approach to healing.
What is a Dual Diagnosis? Unmasking the Connection
A dual diagnosis, or what clinicians call “co-occurring disorders,” is the clinical term for when a person experiences a mental health disorder and a substance use disorder simultaneously. One does not necessarily cause the other, but they are deeply and complexly linked, influencing and exacerbating each other in a cyclical pattern that can feel impossible to escape.
The statistics reveal just how common this overlap is. According to data from the Substance Abuse and Mental Health Services Administration (SAMHSA), millions of adults struggle with co-occurring disorders. The National Alliance on Mental Illness (NAMI) reports that roughly one-third of all people experiencing mental illnesses and about half of people living with severe mental illnesses also experience substance abuse.
Common co-occurring mental health disorders include:
Major Depressive Disorder
Generalized Anxiety Disorder (GAD) and Panic Disorder
Post-Traumatic Stress Disorder (PTSD)
Bipolar Disorder
Attention-Deficit/Hyperactivity Disorder (ADHD)
Eating Disorders
For too long, these conditions were treated in isolation, as if they existed in separate worlds. A person might be sent to rehab for their drinking, while their underlying depression was ignored. Or they might see a therapist for anxiety, while their escalating use of prescription pills remained a secret. This siloed approach is fundamentally flawed because it fails to treat the whole person.

The Intricate Dance: How Addiction and Mental Health Interact
Trying to determine which came first—the addiction or the mental health disorder—is often like asking about the chicken and the egg. The relationship is rarely that simple. Instead, they interact in a powerful, bidirectional loop.
1. The Self-Medication Hypothesis: For many, the journey begins with an attempt to soothe the symptoms of an undiagnosed mental health condition. The crushing emptiness of depression may be temporarily lifted by a stimulant. The racing thoughts of anxiety might be quieted by alcohol.
The intrusive memories of PTSD can be numbed by opioids. In this context, substance use is not a search for a "high," but a desperate attempt to find equilibrium—a way to feel "normal." This self-medication offers a fleeting illusion of control, but it inevitably backfires, often worsening the original symptoms and creating a new, formidable problem: dependency.
2. Substance-Induced Mental Health Issues: Conversely, chronic substance use can significantly alter brain chemistry, structure, and function. The brain’s delicate balance of neurotransmitters like dopamine, serotonin, and norepinephrine is disrupted. Prolonged alcohol use, for example, is a known depressant that can trigger or intensify depressive episodes.
Stimulants like cocaine or methamphetamine can lead to paranoia, psychosis, and severe anxiety. In these cases, what may have started as recreational use can unmask a latent mental health condition or create a new one.
3. Shared Underlying Risk Factors: Often, both disorders stem from common roots. Factors like genetic predisposition, exposure to trauma or chronic stress, and environmental influences can create a vulnerability to both addiction and mental illness.
An individual who has experienced significant childhood trauma, for instance, is at a higher risk for developing both PTSD and a substance use disorder, as both conditions can arise from the same initial wound.
The Flaw of Sequential Treatment: Why One-at-a-Time Fails
The traditional model of care often insisted on treating the "primary" issue first. The logic seemed simple: "Get sober, and then we'll address your anxiety." However, this approach is like trying to repair a boat with two large leaks by plugging only one.
When you treat the addiction without addressing the co-occurring mental health disorder:
Relapse rates are dangerously high. The untreated symptoms of depression, anxiety, or trauma become powerful triggers. When life feels unbearable, the brain’s well-worn pathway of turning to a substance for relief is incredibly difficult to resist.
When you treat the mental health disorder without addressing the addiction:
Therapeutic progress stalls. Substance use can destabilize moods, interfere with the efficacy of psychiatric medications, and impair the cognitive clarity needed to engage in meaningful therapy. A person cannot fully heal from trauma while simultaneously numbing their feelings.
This fragmented care leaves individuals trapped in a revolving door of treatment centers and therapy offices, often feeling more hopeless with each attempt. They are told they are "not ready" for therapy or "not compliant" with rehab, when in reality, the system has failed to see them fully.
Integrated Treatment: The Gold Standard for Dual Diagnosis
True, lasting healing requires a paradigm shift. The most effective, evidence-based approach is integrated treatment, where both the substance use disorder and the mental health condition are addressed simultaneously, by one cohesive team, in one comprehensive plan.
At Anmol Jeevan Foundation, our philosophy is built on this integrated model. It involves:
Comprehensive Assessment: The journey begins with a deep, holistic evaluation to understand the unique interplay between a person’s mental health, substance use, personal history, and wellness goals.
A Unified Team: Our clients are supported by a multidisciplinary team of psychiatrists, therapists, addiction counselors, and medical staff who communicate and collaborate constantly. There are no separate camps; there is one team with one mission: your well-being.
Evidence-Based Therapies: We utilize a blend of therapies proven to be effective for dual diagnosis, such as Cognitive Behavioral Therapy (CBT) to change harmful thought patterns, Dialectical Behavior Therapy (DBT) to build emotional regulation skills, and trauma-informed modalities like EMDR to heal underlying wounds.
Medication Management: When appropriate, our psychiatric team can prescribe and manage medications that treat mental health symptoms, which can in turn reduce the urge to self-medicate and create the stability needed for recovery to take root.
Holistic Healing: We believe recovery extends beyond the clinical. We integrate practices like mindfulness, nutrition, yoga, and purpose-driven activities to help individuals rebuild their lives from the ground up, fostering resilience in mind, body, and spirit.
A Message of Hope for Individuals and Families
If you are reading this and see yourself or a loved one in these words, please know this: you are not broken, and you are not alone. The struggle you are facing is real, it is valid, and it is treatable. A dual diagnosis is not a life sentence; it is a signpost pointing toward the need for comprehensive, compassionate care.
For families, watching a loved one grapple with this can be heartbreaking and confusing. The best way to offer support is through education and empathy. Understand that the irrational behaviors you may be seeing are often symptoms of this dual struggle.
Encourage your loved one to seek integrated treatment, set healthy boundaries to protect your own well-being, and remember that their recovery is their journey to walk—but they don't have to walk it alone.
Healing from co-occurring disorders is a journey of reintegration—of bringing the fractured pieces of yourself back into a cohesive whole. It’s about learning to manage your mental health without a chemical crutch and building a life so fulfilling that the escape offered by substances is no longer needed.
If you are ready to stop treating just one part of the problem and start healing your whole self, we are here. Reach out to Anmol Jeevan Foundation today. A life of clarity, balance, and true wellness is not just possible—it’s waiting for you.




Comments